When a vein is clogged, blood flow is affected, risking potential health concerns. A peripheral venogram, also known as an iliac vein venogram, is an invasive diagnostic test used to provide images of the veins in the legs. The primary purpose is to detect deep vein thrombosis (DVT), or to structurally identify veins. Based on the test results, our physicians may determine the need for venous stenting, a minimally invasive procedure, to widen the narrowed vein, resulting in healthier blood flow.
What is venous stenting?
Stenting is the process of placing a stent. A stent is a tiny wire mesh tube made of medical-grade stainless steel or cobalt alloy metal. Stents expand against blocked or narrowed vein walls and are left there permanently. They act as a scaffold to keep veins open. In most cases, physicians place venous stents in larger, central veins, such as those found in the legs, chest or abdomen.
How is venous stenting performed?
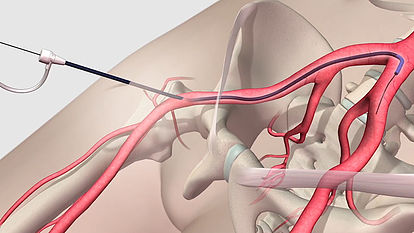
Venous stenting involves the administration of a fine angioplasty catheter into the affected vein. Utilizing advanced imagery technology, one of our physicians will carefully guide the angioplasty catheter where the vein is at its most narrow. A wire with a ballooned tip will be inserted through the catheter where it will widen the narrowed vein, resulting in healthier blood flow. The physician will then remove the angioplasty balloon and insert a catheter with a closed stent on it. He will then place the stent in the vein, which pushes against the walls of the vein, serving as a support to keep it open.
This procedure is minimally invasive, which will not require any extensive incisions.
What can I expect following my venous stenting procedure?
A blood-thinning medicine may be prescribed to you to prevent blood clots and to aid in proper blood flow until the treated area heals. Each patient will have follow-up appointments with our physicians to monitor your recovery process.